Chiropractic, Back Pain, Disc Herniation
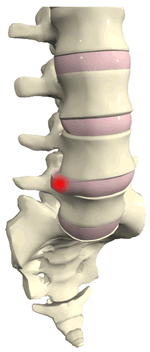
Over the last few years, it has been recognized in the medical literature that conservative treatment works best for many cases of lumbar disc herniation. For patients with far-lateral, or extreme lateral herniation, however, the effectiveness of conservative care is less certain. This recent case study looked at the outcomes of nonsurgical management of a client with far-lateral disc herniation.
The 60-year-old male client was physically active, and had been seen at a Spine Specialty Center previously for treatment for lower back pain, which resolved. 15 months later, he presented at the Center again with severe back pain (present for 3 weeks), with pain radiating to his right buttock and calf.
Presenting Symptoms:
- Score of 73 (out of 100) on the Oswestry Low Back Questionnaire, and Numerical Pain Ratings of 6 (best) to 10 (worst) on a 1-10 scale.
- Difficulty transitioning from sitting to standing
- Altered gait
- Inability to assume erect position
- Lateral list to left
- Asymmetric static pelvic landmarks (right iliac crest 4 degrees high posteriorly, 2 degrees high anteriorly with standing).
- Pain on right side with lateral and backward bends
Initial treatment included manipulation, traction, and passive movements. This was followed up by instruction in self-correction exercises to be followed at home.
Follow-up consisted of:
2 days later: More traction/passive movement and gradual increase in weight bearing, and the patient was fitted with a back brace.
6 days later: manipulation was performed and the patient returned to work part-time. A MRI and surgical consult were also requested during this fourth visit.
The lumbar MRI showed a lateral L5, S1 disc rupture with L5 nerve impingement; due to patient improvement, surgery was deferred. The patient was at work full-time, with his primary complaint sitting intolerance. With consultation, 1 week later a CT-guided transforaminal lumbar epidural and nerve root steroid injection were performed. Three days later, leg pain was reduced and the patient was sleeping better, was working full-time, and was driving.
The patient was then referred to physical therapy for further rehabilitation.
By the end of 4 weeks of physical therapy—8 weeks after being seen initially for the herniation—the patient had achieved scores of 0 on the Numeric Pain Scale, and of 2 (out of 100) on the Oswestry Low Back Pain Questionnaire.
During 2 follow-up visits at 14 weeks and 20 weeks after the initial complaint, all scores were 0. The patient was exercising by running or alternatively using a stair climbing machine with no pain, and continuing his stabilization exercises. He was asymptomatic 1 year later at follow-up.
The study authors also note that this patient responded well to nonsurgical intervention, but was very fit, motivated, and compliant with treatment. The case study did demonstrate the fact that a multi-disciplinary approach to treatment seems most effective: from manipulation and passive motion/traction, to epidural steroid injection once the effectiveness of these first interventions had plateaued, followed up by physical therapy and ongoing exercises.
Erhard RE, Welch WC, Liu B, Vignovi M. Far-lateral disk herniation: case report, review of the literature, and a description of nonsurgical management. Journal of Manipulative and Physiological Therapeutics 2004;27:e3.
